Common retinal problems
- Home
- Current: Common retinal problems
Diabetic Eye Disease
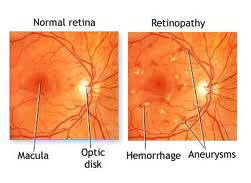
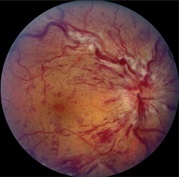
What is Diabetic Retinopathy?
Diabetic Retinopathy is a complication of diabetes, and a major cause of blindness. It is caused by the deterioration of the blood vessels that nourish the retina. These weakened blood vessels may leak fluid or blood, develop fragile brush-like branches, and become enlarged in certain places. Leaking blood or fluid can damage or scar the retina, resulting in blurred vision and, if left untreated, blindness.
Diabetic Retinopathy may be silent or may cause gradual blurring of vision. In advanced cases, there may be sudden onset of floaters, or vision may suddenly become blurred. Probably the most significant treatment of diabetic retinopathy involves the use of laser surgery to seal to photocoagulate the leaking blood vessels. This procedure is done in the office.
Small bursts of laser light energy heat up the small blood vessels and form tiny scars inside the eye. These scars reduce abnormal blood-vessel growth. If diabetic retinopathy is detected early, laser treatment may stop continued damage. Even in advanced stages, laser treatment can reduce the chance a patient will suffer severe vision loss.
How many sittings of laser treatment are required?
It may vary from patient to patient, the severity of diabetic retinopathy and media clarity, generally atleast 3 sittings are required at a week interval.
What are Anti VEGF agents, and what is their role in managing diabetic retinopathy?
Anti VEGF agents (Ranibizumab, Bevacizumab, Ozurdex, Afibercept) are emerging as the new modality of treatment for various stages of diabetic retinopathy. These agents are injected into the eye (intravitreal injection) under anaeshthesia in operation theatre. Injecting the drug takes few seconds. They are commonly used in diabetic maculopathy and proliferative diabetic retinopathy. They may also be used as an adjunct before surgery for diabetic vitreous hemorrhage and retinal detachments.
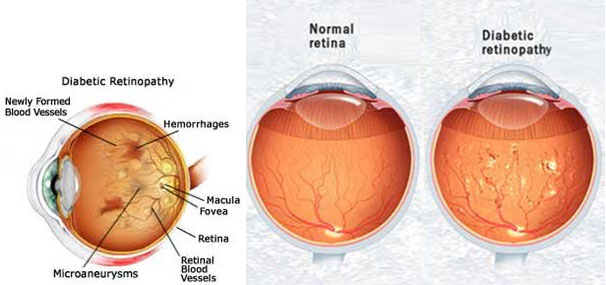
How does diabetic retinopathy damage the retina ?
Diabetic retinopathy occurs when diabetes damages the tiny blood vessels in the retina. At this point, most people do not notice any changes in their vision. Some people develop a condition called macular edema. It occurs when the blood vessels leak fluid and lipids onto the macula, (The central part of the retina that lets us see in detail). The fluid makes the macula swell, thus blurring the vision.
Types of Diabetic Retinopathy:
- Background Diabetic Retinopathy (NPDR), the early stage of D.R. In this stage, tiny blood vessels within the retina leak blood or fluid. Many people with diabetes have mild NPDR, and it does not affect their vision.
- Proliferative Diabetic Retinopathy (PDR), the stage when new abnormal vessels begin growing on the surface of the retina or optic nerve. The main cause of PDR is the widespread closure of blood vessels to the retina, preventing adequate blood flow. The body then responds by growing new blood vessels in an attempt to supply the area where the original vessels closed. PDR causes vision loss in the following ways; vitreous hemorrhage, traction retinal detachment, and neovascular glaucoma.
Retinal Detachment
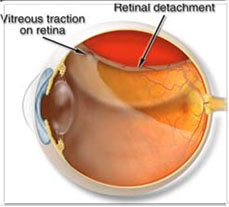
What is a retinal detachment?
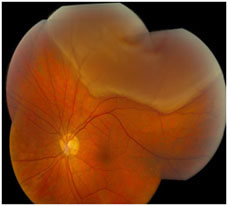
Retinal detachments occur when the retinal is pulled away from its normal position. Once the retina is detached, in no longer works properly. Retinal detachments can lead to blindness is not treated.
What causes a retinal detachment?
The vitreous is a clear gel that fills the eye, with age; the vitreous can sometimes pull away from the retina. Usually when the vitreous separates from the retina there are no complications, but in a small number of people the vitreous can pull hard enough the tear the retina in one or more places. Fluid is then able to pass through the retinal tear/ detachment, lifting the retina off the back of the eye, similar to how wallpaper can peel off a wall.
You may have increased chances of getting a retinal detachment is you have any of the following conditions:
- Nearsightedness
- Previous cataract surgery
- Glaucoma
- Severe eye injury
- Previous retinal detachment in the other eye
- Family history of retinal detachments
- Weak areas in the retina, recognizable by your ophthalmologist
Age Related Macular Degeneration (ARMD or AMD)
What are the symptoms of AMD?
Blurred vision, dark areas or distortion in your central vision, and some times, permanent loss of your central vision. The peripheral vision is usually spared. Early symptoms are loss of clarity while reading and distortion of objects. With advanced macular degeneration you may fail to recognize a person's face. AMD usually affects both eyes, although not necessarily to the same extent.
Dry AMD
With dry macular degeneration, vision loss is usually gradual. These patients need to monitor their central vision regularly. If you notice any change in your vision, you should tell your eye doctor right away, as the dry form can change into the more damaging form which is wet (exudative) macular degeneration. While there is no medication or treatment for dry macular degeneration, some people may benefit from vitamin supplements (anti-oxidants).

Wet AMD
About ten percent of people who have macular degeneration have the wet form. This can cause more damage to your central vision than the dry form. Wet macular degeneration occurs when abnormal blood vessels begin to grow underneath the retina. This blood vessel growth is called choroidal neovascularization (CNV) because these vessels grow from the layer under the retina called the choroid. These new blood vessels may leak fluid or blood, blurring or distorting central vision. Vision loss from this form of macular degeneration may be faster and more noticeable than dry AMD.

Can AMD be prevented?
The exact cause of AMD is unknown. A healthy life style without smoking and a good diet may reduce the risk.
Can AMD be treated?
There is no treatment for dry AMD, although high dose multivitamin combination has been shown to decrease the risk of visual loss. There are a few treatment options for wet AMD although the best outcomes occur when this disease is detected early. These include thermal laser, photodynamic therapy, anti-VEGFs (Lucentis, Avastin, Macugen) or combinations of these. Not all patients may benefit from these, and treatment may not prevent further vision loss.
How will you know you have AMD?
Early reporting of new distortion or blurred vision should be reported to the eye doctor. The earlier the disease is detected, the more amenable it is to treatment. The earliest symptom is distortion of straight lines, making a grid pattern appear distorted.
Floaters and flashes?
What Are Floaters And Flashes?
Floaters are very common and are normally harmless. They are more common if you are short-sighted or as you get older. Some people notice they see flashes of light. These can be due to movement of the gel inside the eye. Very occasionally, flashes or an increase in floaters can be a sign of a retinal detachment, which needs treating as soon as possible
It is important that you get advice as soon as you can if you have:
• a sudden increase in floaters, particularly if you also notice flashing lights
• a new, large, floater
• a change in floaters or flashing lights after you have had a direct blow to your eye
• a shadow spreading across the vision of one of your eyes.
Floaters
Floaters appear as black spots or something that looks like a hair or small pieces of a cobweb. These can be semi-transparent or dark and appear to float in front of your vision. If you have had these for years, your eye and your brain learn to ignore them. Sometimes the number of floaters increases as you get older. Occasionally an increase in floaters can be a sign of problems inside the eye.
Because they 'float' in the jelly of your eye, you will find that if you move your eye to try to look at a floater, it will move away in the direction you move your eye. You might only see the floater if you are staring at a light coloured surface or at the sky during the day.
Some people find that floaters can be a nuisance, but most people become used to them. They rarely cause problems with your vision.
Why do floaters occur?
Some people are born with floaters. Other floaters occur as you get older when the gel in your eye, the vitreous, naturally shrinks. The gel separates into watery fluid and wavy collagen fibrils. The fibrils are seen as line-shaped floaters. Sometimes the gel shrinks enough to collapse away from the retina. Once the gel has collapsed, some people see a large ring-shaped floater.
The collapse of the vitreous gel can pull on your retina. If this happens you would see this as flash of light.
Floaters can also be caused by some eye diseases that cause inflammation.
Who Is At Risk Of Floaters?
Floaters are more common in people who are short-sighted. They may increase if you have had an eye operation such as cataract surgery, or laser treatment after cataract surgery.
What Might Happen If You Have Floaters?
Most of the time floaters are harmless. Sometimes they may be annoying, but treatment is not advised. Occasionally a sudden increase in floaters – either one or more large ones or a shower of tiny ones – may be a sign of a more serious eye disease such as a retinal detachment. This is when your retina pulls away from the back of your eye, and it may lead to a sudden increase in floaters and possibly a shadow in your vision which does not go away. This needs immediate attention.
Flashes
When we are young, the vitreous gel is firmly attached to the back of our eye. As we get older, the vitreous gel naturally becomes more liquid and collapses away from the retina. This is called posterior vitreous detachment (PVD). If you get a PVD you may see flashes of light in front of one of your eyes, like small sparkles, lightning or fireworks. These tend to be in the extreme corners of your vision and come and go but don't obscure any part of your vision. The flashes don't last for a set length of time, and you may notice them more if you go from a light to dark environment. They may continue on and off for weeks or months. These are different to the shimmering or zig-zag lines that may be part of a migraine. Migraine shimmers are a flickering of light, often on only one side of your vision, which then expands to the outside of your vision with a sort of jagged pattern. This will often obscure at least part of your vision (the left or right side). The shimmers usually go away after 10 to 20 minutes and may be followed by a headache, although some people may get migraine shimmers even if they do not have a headache afterwards. Flashes can also occur if you are hit in your eye.
What Might Happen If You Get Flashes?
Sometimes flashes just indicate a tug on your retina and nothing more. However constant flashes may be a sign of a retinal detachment. A retinal tear or retinal detachment may lead to a sudden increase in floaters as well as flashes. You might notice a shadow at the edge of your vision too. This needs immediate attention.
What is retinal vascular occlusion?
The vascular system includes blood vessels called arteries and veins, which transport blood throughout your body, including your eyes. Your retina requires a constant supply of blood to make sure your cells get enough nutrients and oxygen. Blood also removes the waste your retina produces. However, it's possible for one of the vessels carrying blood to or from the retina to become blocked or to have a blood clot. This is called an occlusion.
The occlusion can cause blood or other fluids to build up and prevent the retina from properly filtering light. When light is blocked or fluids are present, a sudden loss of vision can occur. The severity of vision loss may depend on where the blockage or clot occurred.
Retinal vascular occlusion is a potentially serious condition, especially if hardening of the arteries, or atherosclerosis, already exists. It occurs most often in middle-aged and older people.
What Are The Different Types Of Retinal Vascular Occlusions?
There are two types of retinal vascular occlusions
Retinal Artery Occlusion
Blockage of one of the retinal arteries, which are blood vessels that carry oxygenated blood from the heart to your retina. A blockage in the main artery of your retina is called a central retinal artery occlusion. A branch retinal artery occlusion happens when the blockage occurs further along in the smaller branches of your artery.

Retinal Vein Occlusion
Blockage of one of your retinal veins, which are blood vessels that carry deoxygenated blood back to your heart. Retinal vein occlusion is also divided into two types:
• Central retinal vein occlusion (CRVO) is a blockage in the main vein of your retina.
• Branch retinal vein occlusion (BRVO) occurs when the blockage is in a smaller branch of veins throughout the retina.
Blockages in your main vein or artery are often more serious than blockages in your branch veins or arteries.
Causes Of Retinal Vascular Occlusion
The specific cause of vascular blockage or blood clots in the retina is unknown. It may occur when the veins of the eye are too narrow. However, other factors that affect blood flow can put you at a higher risk of having retinal vascular occlusion. These risk factors include:
• atherosclerosis, or hardening of the arteries
• blood clots, which often travel from elsewhere in the body to the eye
• a blockage or narrowing in the carotid arteries of the neck
• heart problems, including irregular rhythm or valve issues
• diabetes
• high blood pressure
• high cholesterol
• being overweight
• intravenous (IV) drug use
• being over the age of 60
• glaucoma, which is a condition that damages your optic nerve
• smoking
• rare blood disorders
• macular oedema, which is fluid build-up, swelling, and thickening of the central part of the retina
• inflammatory disorders such as giant cell arteritis
Symptoms Of Retinal Vascular Occlusion
The primary symptom of retinal vascular occlusion is a sudden, painless change in vision of one eye. This could include blurry vision or a partial or complete loss of vision.
The changes in eyesight could be short term or permanent, depending on how quickly you seek treatment and if you have other health conditions. You should make an appointment with your eye doctor right away if you experience any changes in your vision.
Complications Of Retinal Vascular Occlusion
The condition can occasionally lead to complications and more serious symptoms. Vision may be severely and permanently affected if any of the following complications occur:
Macular edema is a swelling in the macula, or the central part of your retina, due to a build-up of blood/fluid.Neovascularization is an abnormal growth of blood vessels caused by poor blood flow and a lack of oxygen to your retina.
Neovascular glaucoma involves fluid build-up and high pressure in your eye. This is a serious complication. It's associated with severe vision loss and possibly loss of the eye.
Retinal detachment is rare. It's a separation of your retina from your eye tissue.
Diagnosing Retinal Vascular Occlusion
Your ophthalmologist will perform a comprehensive exam to diagnose retinal vascular occlusion. They'll check your vision, pressure within your eyes, and the physical appearance of your eyes. Your doctor will assess your eye function and the look of the pupil. They may also measure your blood pressure and suggest a blood test to check for blood clotting conditions.
The following eye tests may also be done:
• Dilated fundus examination.
• Optical coherence tomography (OCT) can be used to take a high definition image of your retina.
Your doctor may suggest other heart tests if they suspect blood clots are coming from somewhere else in your body. These tests may include an echocardiogram, electrocardiogram, colour doppler, cholersterol levels and a heart monitor to check your heart's rhythm. These tests will assess your heart and vascular system.
Preventing Retinal Vascular Occlusion
The best way to prevent retinal vascular occlusion is to identify and treat the risk factors. Since retinal vascular occlusion stems from vascular issues, it's important to make lifestyle and dietary changes to protect your blood vessels and keep your heart healthy. These changes include:
• exercising
• losing weight or maintaining a healthy weight
• eating a healthy diet low in saturated fat
• not smoking or quitting smoking
• controlling diabetes by keeping your blood sugar at a healthy level
• taking aspirin or other blood thinners after consulting with your physician first
Routine checkups with your doctor can help you learn whether or not you have any of the risk factors of retinal vascular occlusion. For example, if your doctor discovers you have high blood pressure or diabetes, you can start preventive treatment right away.
Treating Retinal Vascular Occlusion
There's no medication available that's specific for retinal artery occlusions. Most people with this condition will have permanent changes to their vision.
To treat retinal vascular occlusion, your doctor may recommend medication such as blood thinners or injections into the eye.
Medications used to treat retinal vein occlusion include:
• Antivascular endothelial growth factor (anti-VEGF) drugs such as Ranibizumab, Bevacizumab and Aflibercept which are injected into the eye
• Corticosteroid drugs that are injected into your eye to control the swelling
In some cases, laser therapy can be used to break down the blockage in the blood vessels and to keep more damage from occurring.
It's possible to develop a blockage in your other eye. Your doctor will develop a prevention plan for you if they're concerned that your other eye is at risk.
What Is Retinopathy of Prematurity?
Retinopathy of prematurity (ROP) is an eye disease that can happen in premature babies. It causes abnormal blood vessels to grow in the retina, and can lead to blindness if left untreated. RETINOPATHY OF PREMATURITY IS A PREVENTABLE CAUSE OF BLINDNESS IN CHILDREN IF DIAGNOSED AND TREATED IN TIME
What Happens in ROP?
Retinopathy of prematurity makes blood vessels grow abnormally and randomly in the eye. These vessels tend to leak or bleed, leading to scarring of the retina, the layer of nerve tissue in the eye that lets us see. When the scars shrink, they pull on the retina, detaching it from the back of the eye. Because the retina is a vital part of vision, its detachment will cause blindness.
How Is ROP Treated?
Some cases of ROP are mild and correct themselves, but others progress to scarring, pulling the retina away from the rest of the eye. These cases require retinal lasers, intravitreal injections of Anti VEGF drugs or surgery, in extreme cases,to prevent vision loss or blindness. ROP laser treatment stops the growth of abnormal blood vessels. Treatment focuses on the peripheral retina (the sides of the retina) to preserve the central retina (the most important part of the retina). ROP laser involves scarring areas on the peripheral retina to stop the abnormal growth and eliminate pulling on the retina. Because treatment focuses on the peripheral retina, some amount of peripheral vision may be lost. However, by preserving the central retina, the eye can still do vital functions like seeing straight ahead, distinguishing colors, reading, etc.

What Is Vitrectomy
The vitreous is removed, therefore the name "Vitrectomy". The lack of vitreous does not affect the functioning of the eye. Saroya Eye Hospital has the latest and sophisticated surgical equipments. Micro incision and sutureless (23/25 gauge) vitrectomy(MIVS) is performed using Retikare Vitrectomy machine.
The surgeries performed in our department are as follows
- Scleral Buckling
- Vitrectomy for retinal detachments, epiretinal membrane, macular hole,vitreomacular traction, vitreous hemorrhage, parasitic cysts, dislocated nucleus, dislocated intra ocular lens
- Vitrectomy for diabetic retinal detachment
- Scleral fixated IOLs
- Surgery for trauma-related conditions
- Surgery for intra ocular infections
- Pneumoretinopexy
About Us
Saroya Eye Hospital Maximizing the visual potential of each of the patients through quality treatment is the mission of Eye-Care Hospital. We are dedicated to providing a positive experience for our patients through thorough professionalism, positive attitude and efficient teamwork
Get Appointment